Predictive analytics is a driving force of modern-day medicine. The technique enables more personalized healthcare, which it does in several ways. Whether through data mining electronic healthcare records, health surveys, or medical alert services, there’s plenty you can do with predictive analytics.
So — if you want to know:
- How predictive analytics can enable effective personalized healthcare
- The most popular predictive models around today
- The key challenges of using the technique
Then this is the article for you.
Ready? Let’s go.
AI In Healthcare Is Already Commonplace
Deploying AI in healthcare is nothing new. A report by Sage Growth Partners shows 90% of healthcare payers and providers with $800m+ annual turnover are proactively exploring AI and automation.
One of the key applications of AI in medicine is predictive analytics, with 60% of practitioners already using this solution. So you can see the technique is popular, but how does it work?
Let’s start there.
| Want a real-world example? See How Artificial Intelligence Is Transforming Diabetes Care |
What Is Predictive Analytics?
“Predictive analytics is a discipline where computer programs analyze past events, occurrences, or patterns to forecast the future in a logical way.”
— Shemmy Majewski, DLabs CEO
Doctors typically lean on experience when prescribing medicines, basing treatments and doses on visible or reported symptoms.
The process is effective, but it’s not without its challenges.
You see, a practitioner will struggle to predict what other infections a patient might be vulnerable to — whereas a statistical approach, like predictive analytics, can analyze historical data to suggest more personalized healthcare advice for any given patient.
The predictive models work by anticipating a patient’s future conditions given their existing symptoms and associated data points. The insights then help practitioners to devise a tailored care strategy at both an individual and patient-cohort level.
All this is made possible thanks to predictive algorithms and training models that can analyze data silos across extensive sources, spanning:
- Electronic Health Records (EHR)
- Administrative Data
- Health Surveys
- Claims-based Datasets
- Medical alert services
- Patient Registries
- Disease Registries
So if you’re still wondering why we need a computer to do this in place of a doctor, there’s your answer.
While doctors can tap their experience to assess a patient, there are limitations in how much data any one person can process. On the other hand, a data-driven technique rules out this shortcoming, enabling more robust patient care at an unbelievable scale and speed.
Moreover, there’s less risk of inherent biases influencing treatment decisions (and not forgetting, we humans are all prone to error!).
The Importance Of Predictive Analytics
Let’s now turn to a story to highlight the importance of predictive analytics. The patient in question is one, Eric Dishman, who needed treatment for kidney cancer.
Eric’s kidneys were failing.
He had fought a rare form of kidney cancer for 23 years but was quickly running out of options. Dialysis was not available to him because he was going through chemotherapy, radiation, and immunotherapy treatments.
Unfortunately, he wasn’t a good candidate for a transplant either. But he is alive and now serves as the CIO at ALL OF US: a $1.5 billion precision medicine initiative to build the world’s largest and most diverse patient dataset. But what saved him?
Doctors put him on pancreatic cancer treatment, and it worked.
And therein lies the need for predictive analytics.
Yes, Eric had kidney cancer. But on the advice of a colleague, he went through genome sequencing.
It turned out his kidney cancer resembled pancreatic cancer more than renal. Meaning the $6m he had spent on kidney treatments over the previous 23 years hadn’t helped his cause. Fast forward to today, Eric asks:
“When I think about the suffering I went through, what if I had gotten it right the first time?”
Predictive Analytics: Use Cases In Healthcare
Data is helping healthcare providers prevent rapid health deterioration as much as intervene at a time that counts.
Thanks to a surge in IoT-powered biomedical sensors, there’s as much as 2,314 exabytes of healthcare data available for analysis today. And that fact alone is helping practitioners answer questions like:
- What are the chances this Cancer patient will recover if s/he is subjected to stem cell transplant or hormone therapy?
- What are the chances this newborn baby will develop sepsis?
- Will this general ward patient deteriorate further and need admission to ICU in the next 48 hours?
- How many extra beds will I need to serve a rising number of patients in the second wave of a Novel Coronavirus virus?
| Extra reading: How Technology Can Improve the Medicine: Machine Learning Methods Used to Detect Cervical Cancer |
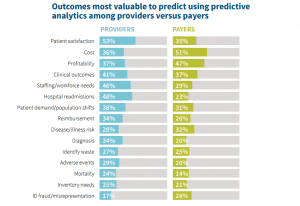
But organizations are deploying predictive analytics across healthcare. The following table shows where both providers and payers find value in the technique.
Source:SOA
But let’s look at some specific examples.
Predicting Patient Health Deterioration
Overstrained intensive care units (ICU) worldwide shift patients who score low on perceived risk parameters to general wards.
The process enables ICUs to provide better care to high-risk patients. The problem is: if a ‘low-risk’ patient moves from ICU to a general ward and contracts a hospital-acquired infection (HAI), their health can rapidly deteriorate.
Worryingly, nursing teams rarely have the capacity to spot the early warning signs and subtle cues of an HAI, while the failure to act for a prolonged period can result in critical events, even death.
But if wards can deploy wearable biosensors (like medical IoT devices/sensors), they can collect, store, and analyze patient physiological and biochemical profiles in real-time, monitoring vitals like the respiratory rate and the heart rate.
The sensors also capture contextual parameters, like a patient’s posture, activity level, and ambulation, combining these data points with machine learning algorithms to determine and predict the early warning scores (EWS) for every patient.
Based on the EWS, a predictive analytics-powered application can trigger notifications to caregivers allowing them to intervene as necessary. And early action can often prevent a patient from having to return to ICU.
One research paper illustrates how predictive analytics help reduce:
- The mortality rate from 45% to 24%
- Cardiac arrest counts by 80%
While at Ysbyty Gwynedd hospital, the team observed a 35% reduction in critical event occurrences and an 86% reduction in cardiac arrests after deploying a predictive analytics solution.
Personalizing Medication Dosages
Traditionally, medicine has been one-size-fits-all. But paradigms are shifting.
Today, it’s possible to leverage technologies like high throughput sequencing, microfluidics, mass spectrometry, and imaging, then turbocharge them with analytics to gain detailed insights into the molecular and cellular alterations of an underlying disease.
By integrating molecular data with anatomical, physiological, environmental, and lifestyle data, then feeding it to predictive models, clinicians can predict and anticipate the best treatments, even personalizing dosages to individual patients.
Given that upwards of 6% of hospital readmissions result from adverse reactions to medication, this could be a step-change in prescriptions.
Avoiding Equipment Downtime With Predictive Maintenance
Medical equipment failure will likely be disastrous. So there’s enormous value in monitoring devices for signs of potential malfunction.
In doing so, maintenance teams can stay on the front foot by fixing a device before it breaks, avoiding disruptions to workflows and patient care. But prognostics require real-time data collected by sensors and actuators that track machine performance.
While the manufacturing year, make and model, warranty, maintenance history, and repair logs fill in the gaps, giving the big picture of a machine’s overall health.
Take an MRI scanner as an example.
These devices degrade with each use. So hospitals deploy sensors that track critical data and flag when a component needs replacement or repair. The solutions can even schedule maintenance automatically, notifying all stakeholders.
Which is why some predict a future of digital twins in which every device has a digital replica, tracking its health and reporting on its maintenance needs.
Reducing Readmission Through Improved Patient Care
Almost 20% of US healthcare expenditure comes from inefficient care resulting in patient readmission. In contrast, an analysis of over 700,000 surgeries suggests that a more predictive, prescriptive approach reduces 30-day hospital readmissions by as much as 12%.
That’s because predictive analytics applications can identify patients exhibiting traits that signal potential readmission, triggering practitioners to assign more personalized care and discharge plans and so minimizing the risk of rapid readmission.
Elsewhere, the Huntsville Hospital in Alabama has used predictive analytics in tandem with clinical decision support (CDS) tools to decrease sepsis mortality among younger, older, and chronically ill patients by as much as 53%.
Personalizing Healthcare For At-risk Individuals And Cohorts
Predictive analytics isn’t only applicable at the individual level. Healthcare providers can use it for population health management as well.
This applies to predicting the failure-success probability of surgery as much as to identifying cohorts exposed to a possible disease outbreak. You can leverage predictive analytics almost anywhere in the healthcare value-chain, uncovering actionable clinical intelligence.
Today, it’s even possible to deliver predictive care in the comfort of the home: great for those suffering from a chronic disease or for higher-risk elderly patients.
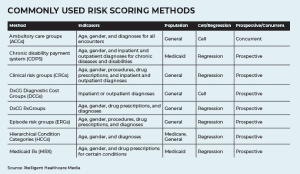
Source: XHM
Applications calculate risk scores by taking data from lab tests, wearable IoT devices, biometrics, and social determinants and identifying people with a heightened risk of developing life-threatening chronic diseases.
The approach allows healthcare providers to intervene at the right time and offer effective personalized care, hopefully preventing longer-term complications.
A study by Mental Health Research Network (MHRN) successfully harnessed EHRs and other clinical intelligence tools to spot individuals with a higher suicide risk, finding 48% of suicide attempts come from the top 5% of those scored as ‘high risk.’
And the applications don’t end there — here are several other ways to use the benefits of predictive analytics in healthcare:
- Avoid no-shows: predict when a patient might not turn up for an appointment, scheduling reminders, offering transport, and suggesting alternative dates.
- Predict busy times: and allocate extra resources when you know your clinic will be full, then flatten the curve by moving appointments, ultimately, reducing waiting times.
Source: Healthitanalytics
- Stay safe from cyberthreats: the Institute for Critical Infrastructure Technology (ICIT) shows you can mitigate the threat ransomware poses to medical data.
- Avoid surgical complications: data can even help prevent surgical complications, potentially saving healthcare providers up to $23 Billion.
The Challenges Of Predictive Analytics
Source: SOA
As you can see, predictive analytics offers plenty of value — for providers, payers, and most importantly, patients. But that’s not to say it’s without its challenges.
Here are the biggest headaches it poses today.
Data Privacy
The more data an algorithm has, the more accurate its predictions will be. But predictions can require data to be shared with third parties, which poses a risk in itself. Moreover, a 55% spike in healthcare-related cyberattacks in 2020 highlights another big healthcare challenge.
In-built Bias
People trust algorithms to be impartial. But the fact is: people build them, so they’ll never be bias-proof. What can make matters worse is a lack of regulation and no real accountability, intensifying the ethical debate.
Moreover, unless people remove potential biases, they’ll only become more acute as predictive models refer back to past decisions.
Moral Hazard
If a doctor believes an algorithm will correct any mistake, there’s a risk the doctor won’t be as concerned about making a mistake in the first place. Moreover, if someone can blame an error on an algorithm, it reduces accountability, potentially increasing the risk even further.
Data Collection
Healthcare organizations rely on multiple EHRs, independent imaging devices, labs, and a colossal volume of unstructured data (like medical notes, drug prescriptions, medical service alerts, and research reports), which presents a considerable challenge in itself.
It’s no easy feat extracting data from various sources, then structuring it in such a way that a machine learning algorithm can make sense of the inputs.
The Healthcare Revolution Has Just Begun
Predictive analytics has three central uses in healthcare: personal care, cohort treatment, and intelligent operational management.
The global analytics healthcare market is projected to surpass $28.94 billion by 2025. But we’re only at the beginning. As IoT unlocks deeper insights into human health, we’ll gain access to yottabytes of medical data.
And we’ll then be able to train algorithms to become more sophisticated and more accurate. Time will tell how authorities respond to the digital disruption, but one thing is clear.
Predictive analytics is all set to transform healthcare.
Interested in learning how AI can give your organization a helping hand? Schedule a free 20-minute consultation with a DLabs.AI expert today.